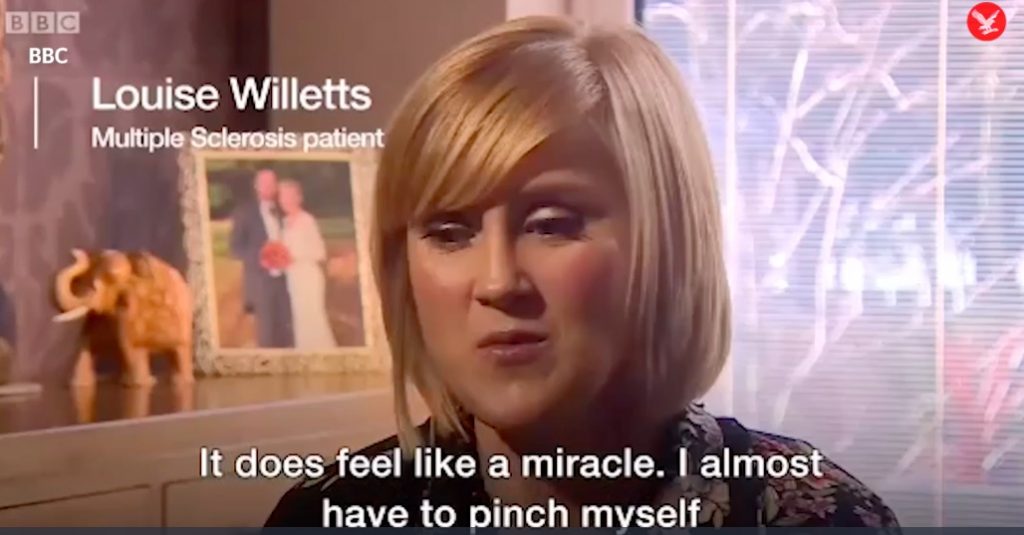
Stem Cell Treatment Has ‘Miraculous Effect’ on MS Sufferers
One ecstatic stem cell recipient and former multiple sclerosis patient raves:
‘It does feel like a miracle. I almost have to pinch myself and think “Is this real l? Is it really gone, is it ever going to come back?”‘
Doctors are hailing a new stem cell treatment for the degenerative disease multiple sclerosis, after trials showed it to reboot patients’ immune systems, halting the disease.
Patients said the results were “a miracle” and had seen them return to normal life after the disease left them in a wheelchair or unable to read.
How To Identify Your Pain
 As a physician dedicated to managing peoples’ pain, one of my most important duties is to accurately identify the type of pain a patient is experiencing, and then recommend the most effective course of treatment.
As a physician dedicated to managing peoples’ pain, one of my most important duties is to accurately identify the type of pain a patient is experiencing, and then recommend the most effective course of treatment.
Because you are reading this blog about pain, there’s a likelihood you are experiencing some level of pain right now, or are anticipating recurring pain. Depending on its location and severity, that pain might be causing you discomfort, distress or even agony. The pain might be steady and constant; in which case, it could be an ache. It might be a throbbing pain or a pulsating pain. It might have a pinching sensation, or a stabbing one.
Pain is a very individual experience, so only the person who is experiencing it can describe the sensation accurately. I’m presenting this basic pain guide to help you understand the different types of pain we have all felt at one time or another. It is not meant to help you diagnose your condition, or to suggest a treatment. It is purely for your information. If you have concerns about your pain or it is extreme or long-lasting, and it hasn’t been responding to home care and over-the-counter medication, please contact a physician for a professional diagnosis.
In follow-up blogs, I’ll write about how pain is measured, and the various treatments offered by the medical community.
Types of pain
Acute Pain – This is an intense and short-lived pain, that could be an indication of an injury. If it is, when the injury heals, the pain usually goes away.
Chronic Pain – Mild or intense, chronic pain lasts much longer than acute pain.
Classifications
Nociceptive Pain – Specific pain receptors are stimulated and sensitive to hot/cold temperature, vibration, stretching, and chemicals released by damaged cells.
Somatic Pain – Generally sharp and very localized, if the affected area is touched or moved, it will hurt more. This pain might be felt on the skin, or in muscles, joints, bones, and ligaments – known as musculoskeletal pain. With somatic pain, pain receptors are sensitive to temperature (hot/cold), vibration and muscle stretch. They are also sensitive to inflammation, which could be from a cut or a sprain that causes tissue damage.
Visceral Pain – Felt in the internal organs and main body cavities, which are divided into the thorax (lungs and heart), abdomen (bowels, spleen, liver, and kidneys), and the pelvis (ovaries, bladder and the womb). The pain receptors are sensing inflammation, stretching and/or oxygen starvation (ischemia).
Visceral pain is more likely to be a vague deep ache that is harder to pinpoint than somatic pain. Colicky and cramping sensations are often types of visceral pain. It commonly refers to some type of back pain – lower, abdominal, mid back, or upper back.
Nerve Pain/Neuropathic Pain – Nerve pain is also called neuropathic pain. It comes from within the nervous system itself and is often referred to as a pinched nerve, or trapped nerve. The pain can originate from the nerves between the tissues and the spinal cord, and the nerves between the spinal cord and the brain (this is known as the central nervous system).
When a nerve is injured it becomes unstable, which causes its signaling system to act haphazardly. The brain interprets these abnormal signals as pain. This chaos can cause other unpredictable sensations, such as numbness, pins and needles, tingling and hypersensitivity to temperature, vibration, and touch.
Neuropathic pain can be caused by nerve degeneration, for example, from a stroke, multiple sclerosis, or oxygen starvation. It could be due to a trapped nerve, which creates pressure on the nerve. A torn or slipped disc will cause nerve inflammation, which will result in neuropathic pain. A nerve infection, such as shingles, can also cause neuropathic pain.
Sympathetic Pain – The sympathetic nervous system controls blood flow to the skin and muscles, perspiration, and how quickly the peripheral nervous system responds. The pain usually occurs with a fracture or a soft tissue injury of the limbs. Much like neuropathic pain, the nerve is injured, becomes unstable and fires off random, chaotic, abnormal signals to the brain, which interprets them as pain.
In general, with this kind of pain the skin and the area around the injury become extremely sensitive and, often, the pain becomes so intense the sufferer doesn’t want to use the hurting arm or leg. Over time, this can cause other problems, like muscle wasting, osteoporosis, and stiff joints.
Referred Pain/ReflectivePain – This is pain felt either nearby or at a distance from the origin of an injury. Good example: during a heart attack, the affected area is the heart, but the pain is often felt in the arms, shoulders, back and neck, rather than in the chest. Doctors have been aware of referred pain for centuries, but researchers have not been able to identify what causes it.
Look for my upcoming blogs on how pain is measured and range of available treatments. Remember, if you are experiencing pain that concerns you, call your physician, or contact the Bram Center for Regenerative Medicine to discuss an expert evaluation.
How Doctors Measure Pain
 In my recent blog on identifying pain (see preceding article), I promised a follow-up on measuring pain. This is a challenge for many practitioners because only the person with the pain can actually feel it, and every individual perceives pain differently. Unfortunately, there is no widely-accepted device that can measure pain accurately. When you’re not feeling well, a thermometer can quickly read your temperature. If you have hypertension, your blood pressure can be checked at a medical office, pharmacy, or even at home. Pain is not so cut and dried.
In my recent blog on identifying pain (see preceding article), I promised a follow-up on measuring pain. This is a challenge for many practitioners because only the person with the pain can actually feel it, and every individual perceives pain differently. Unfortunately, there is no widely-accepted device that can measure pain accurately. When you’re not feeling well, a thermometer can quickly read your temperature. If you have hypertension, your blood pressure can be checked at a medical office, pharmacy, or even at home. Pain is not so cut and dried.
Communication is vital
If you schedule an appointment to have a pain issue diagnosed, take a moment to make a detailed list before you go, including:
- When you first felt the pain
- The affected body area
- The characteristics of the pain– throbbing, acute, vague, etc.
- What triggers it/what relieves it
- Symptoms other than the pain
- And any other information that could be relevant.
Also, keep track of your pain in a diary or journal, and bring it along too. This will give your doctor a better understanding of your pain so he or she can diagnose and treat it.
Pain scales help
Some healthcare professionals use pain scales to assess current pain and whether any medications you might be taking are helping. There are different pain scales for infants, children, adults and patients with difficulties communicating.
A pain scale usually includes a range of choices to help express different intensities. It might feature numerals or illustrations of pained faces, from smiling to crying. For example, “How bad is your pain right now on a scale from 0 to 10, with 0 being no pain and 10 being the worst pain ever?”
There are also tests that some doctors administer to get a better picture of a patient’s pain by identifying its cause:
- X-rays produce images of the body’s internal structures and can detect broken bones and joint problems
- Electrodiagnostic procedures, like electromyography (EMG), nerve conduction studies, and evoked potential (EP) studies, can show which muscles or nerves are affected by weakness or pain
- Imaging, especially Magnetic Resonance Imaging (MRI), provides pictures of the body’s structures and tissues. Magnetic Resonance Imaging uses magnetic fields and radio waves to differentiate between healthy and abnormal tissue
- A neurologic exam can test a patient’s movement, reflexes, sensation, balance and coordination, and reveal a nerve problem.
The aim of all these tools is to assess your pain as accurately as possible so your doctor can diagnose your condition and recommend a pain management solution that works best for you – treatments such as Platelet Rich Plasma and Stem Cell Therapy.
At the Bram Center for Regenerative Medicine, we perform interventional and minimally-invasive procedures to help relieve painful conditions. If you’re experiencing acute or chronic pain that hasn’t been responding to home care and over-the-counter medication, contact us today to find out more about an expert evaluation. Dr. Harris Bram and his elite staff will devote the necessary time make you feel comfortable and confident that you’re in experienced and caring hands.
4 Basic Benefits Of PRP Therapy For Pain Management
 Platelet Rich Plasma (PRP) is one of the effective treatments offered at the Bram Center for Regenerative Medicine. PRP Therapy a fast, simple, non-invasive procedure that provides superior relief for acute or chronic pain by promoting the natural healing potential of the body. It accomplishes this by using platelets from your own blood.
Platelet Rich Plasma (PRP) is one of the effective treatments offered at the Bram Center for Regenerative Medicine. PRP Therapy a fast, simple, non-invasive procedure that provides superior relief for acute or chronic pain by promoting the natural healing potential of the body. It accomplishes this by using platelets from your own blood.
If you have a tendon, ligament and joint injury that hasn’t responded to traditional treatments, you might want to learn about PRP Therapy.
For starters, here are four basic advantages:
PRP Therapy is Safe
Because the procedure uses platelets harvested from your own blood, there is no risk of disease injection or transmission. There is also no risk of allergic reaction or rejection.
PRP Therapy is Convenient
It does not involve complex surgical procedures. Your pain management doctor simply extracts platelets, plasma and any other needed cells to customize the optimum formula for your specific needs.
PRP Therapy is Natural
Because this treatment uses your own platelets, your body doesn’t feel any sense of being violated by foreign matter. As a result, your system won’t act to reject it. Platelet Rich Plasma Therapy simply enables your body to heal itself naturally.
PRP Therapy is Cost Efficient
Because all the necessary components for healing are taken directly from your body, and the one-hour process is done right in our medical center, it can avoid running up a hospital bill.
Interested? We are eager to tell you more about Platelet Rich Plasma Therapy and how it can work for you. Our doctors have extensive experience using PRP to treat a variety of tendon, ligament and joint injuries. These include rotator cuff injuries, tennis elbow, Achilles’ tendon, plantar fasciitis, meniscus tears, bursitis of the hip, knee pain or ligament sprains.
Please contact our nearest office to discuss whether you’re a good candidate for this remarkable procedure.
At the present time, Platelet Rich Plasma treatments are not covered by medical insurance.
Painkillers: The Difference Between Opiates & Opioids
 One of the most frequent reasons people visit their family doctor is to get relief from pain. If an over-the-counter pain reliever isn’t working to their satisfaction, the doctor can prescribe a stronger pain medication. Unfortunately, when it’s not taken according to the doctor’s instructions, or it’s used for an extended period of time, this stronger drug can lead to addiction.
One of the most frequent reasons people visit their family doctor is to get relief from pain. If an over-the-counter pain reliever isn’t working to their satisfaction, the doctor can prescribe a stronger pain medication. Unfortunately, when it’s not taken according to the doctor’s instructions, or it’s used for an extended period of time, this stronger drug can lead to addiction.
A study released earlier in 2016 revealed that almost half of all Americans personally know someone who has been addicted to prescription meds – opiates or opioids. As a pain management specialist, I’ve found that many people aren’t clear on the difference between these two types of drugs. So, for your information, whether you someday need to discuss them with a health care professional, family member or friend, here’s a brief overview.
Opiates – A Natural Pain Medication
Opiates are derived from the opium poppy. Opium is a strong pain-relieving medication used in different opiates:
- Morphine
- Codeine
- Heroin
- Opium
Opioids – Synthetic Pain Remedy
Opioids are synthetic or partly-synthetic drugs that are manufactured to work in a similar way to opiates:
- Methadone
- Percocet, Percodan, OxyContin (oxycodone)
- Vicodin, Lorcet, Lortab (hydrocodone)
- Demerol (pethidine)
- Dilaudid (hydromorphone)
- Duragesic (fentanyl)
How Opiates And Opioids Work
Both types of painkillers don’t actually “kill” the pain – they alter the way the pain is perceived. They attach onto opioid receptors in the brain, which send inaccurate measures of the severity of the pain that the person is experiencing. So, it actually feels like less pain than it would if the brain wasn’t being tricked.
(These powerful drugs are popular for another reason too: People who are not in pain take them because they affect how the brain perceives pleasure. They provide a feeling of elation, followed by deep relaxation and/or sleepiness.)
Addiction To Opiates And Opioids
When people use opiates and opioids to treat pain as directed and for a short time, they are less likely to become addicted. Addiction occurs when patients develop a tolerance for the level of medication they have been described and no longer get the same level of relief. So they take more and more. And they just can’t stop without help.
Before It’s Too Late
If you’re at a point where an over-the-counter or prescription pain medication is not working for you – or you’re getting concerned about how much you’re taking, please contact the Bram Center for Regenerative Medicine for a consultation with one of our elite pain management doctors. We offer a variety of interventional and minimally-invasive procedures – including Stem Cell Therapy and Platelet Rich Plasma (PRP) – that can help relieve your pain without dangerous drugs, surgery and a lengthy recovery.
At the present time, Platelet Rich Plasma and Stem Cell treatments are not covered by medical insurance.
Dr. Bram Named “Top Doc” By Leading Rating Firm
 Castle Connolly Medical Ltd, is the nation’s most trusted source for identifying top doctors. Every year Castle Connolly surveys hundreds of thousands of physicians and asks them to nominate other physicians whom they believe to be among the very best in their specialty or specialties in their communities across the nation. In addition to its online nomination process, Castle Connolly’s physician-led research team makes thousands of phone calls to identify excellent doctors and reinforce the survey process.
Castle Connolly Medical Ltd, is the nation’s most trusted source for identifying top doctors. Every year Castle Connolly surveys hundreds of thousands of physicians and asks them to nominate other physicians whom they believe to be among the very best in their specialty or specialties in their communities across the nation. In addition to its online nomination process, Castle Connolly’s physician-led research team makes thousands of phone calls to identify excellent doctors and reinforce the survey process.
This year Castle Connolly has selected Dr. Harris Bram to the Top Doctors New York Metro Area: 2017 edition. The Top Doctors in the NY Metro Area represent the top 10% of doctors in a twenty-county area spanning New York, New Jersey and Connecticut. Physicians do not and cannot pay to be included in any Castle Connolly guide or list.